Change is inevitable, and the only constant. Adopting electronic business transactions will increase significantly as more and more organizations in the health space aim at cost savings. As per the latest CAQH Index report, digital health technologies’ adoption stood at 6% for the medical and 4% dental industry. HumaneBITS have taken a dig at various industry studies and have tried to analyze a crucial functional area that is more likely to impact cost over the long term.
Administrative function is an essential component in healthcare to ensure quality patient care and ensure that the providers are compensated adequately and timely for the care provided. The first step in the process is provider enrollment. While the CAQH report has provided a lot of emphasis on the administrative cost associated with the business’s patient side, HumaneBITS has been trying to reduce administrative wastage from a provider’s perspective.
Provider Enrollment is challenged by the volume and variability of payer enrollment forms. Additional challenges include a lack of automation, not optimizing available electronic solutions, and obtaining and maintaining provider data. Healthcare organizations continue to experience last-minute notification of providers’ start dates. A recent survey respondent stated that one-third of the time, they receive only a 30-day notice of a provider’s start date, which results in a reprioritization of current work.
Need for Inter-Operability between Payers and Providers
- Create a single port of entry for submission of provider credentialing, privileging, and enrollment applications as well as provider changes. This port of access should be defined and supported by a system policy and procedure.
- Collect at one time from providers the data needed to complete the organization’s credentialing, privileging, enrollment, and health plan requirements.
- Submit Medicare enrollment and changes using the electronic PECOS database.
- Optimize the software solution used to pre-populate provider enrollment forms and credentialing applications.
- Cross-team Collaboration between Recruitment and Human Resources to develop workflows to ensure timely notification of new providers.
Why is it a time to change? Working with a Digital Health Technology firm will help overcome some of the challenges mentioned below from a business standpoint.
Reduce the turnaround time
Turnaround time has a high impact on your revenue cycle Management. Automation should reduce the turnaround time and help you get the provider started on with the patients quickly. Especially around the times like the Pandemic & COVID-19, remote working is the new norm. Now is the ideal time for clearinghouses and RCM partners to examine their enrollment programs. The key to reducing the turnaround time is to include providers directly in the process. It cut back on middle layers, reduce mistakes due to manual data handling and make use of your data. It also auto populate forms using automated data collection from providers’ payers, thereby automating the whole process.
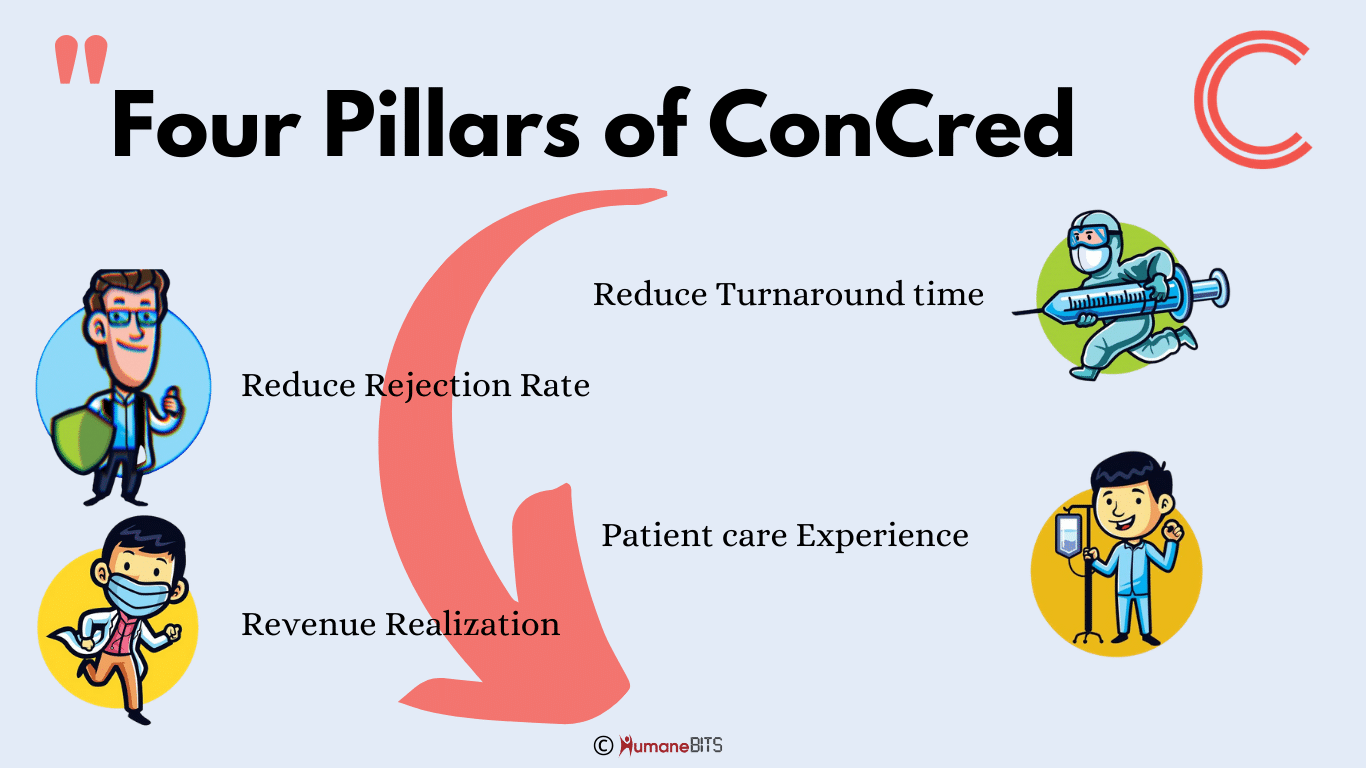
Rejection Rate
Along with speed, the system that you choose must be accurate. Accuracy is the key to reducing the claims rejection rate. It is an important area where interoperability between the payer and the provider plays a critical role. ConCred is an Integrated Contracting and Credentialing system along with the services team at HumaneBITS, has more than ten-man years of experience in the healthcare domain.
Revenue Realization
Time is money, and any delay in enrollment directly impacts revenue as this will delay the provider from starting to see the patients.
Improve Patient Care Experience
If it is not measurable, it is not doable. While the ultimate payer being the patient, providing an experience to your customers is the most critical aspect of your healthcare business to maximize revenue.
ConCred’s single source of truth dashboard makes it seamless for you to track using alerts and notifications to take the corrective measures on time and avoid delays and improve the ultimate patient care experience.
For more details or to schedule a demo, please write to contact@humanebits.com